Intensive Outpatient Programs: 7 Ways IOPs Support Your Mental Health and Addiction Recovery



Dr. Glowiak has a PhD in counselor education and supervision and has served those struggling with addiction while continuing to spread awareness on the topic to students, clinicians, instructors, and the general public.




Dr. Glowiak has a PhD in counselor education and supervision and has served those struggling with addiction while continuing to spread awareness on the topic to students, clinicians, instructors, and the general public.
In the journey toward recovery, individuals facing mental health and addiction challenges often encounter a crossroads filled with uncertainty and fear. One promising path that has emerged in recent years is the intensive outpatient program (IOP), a supportive bridge between the structured environment of inpatient care and the freedom of traditional outpatient treatment.
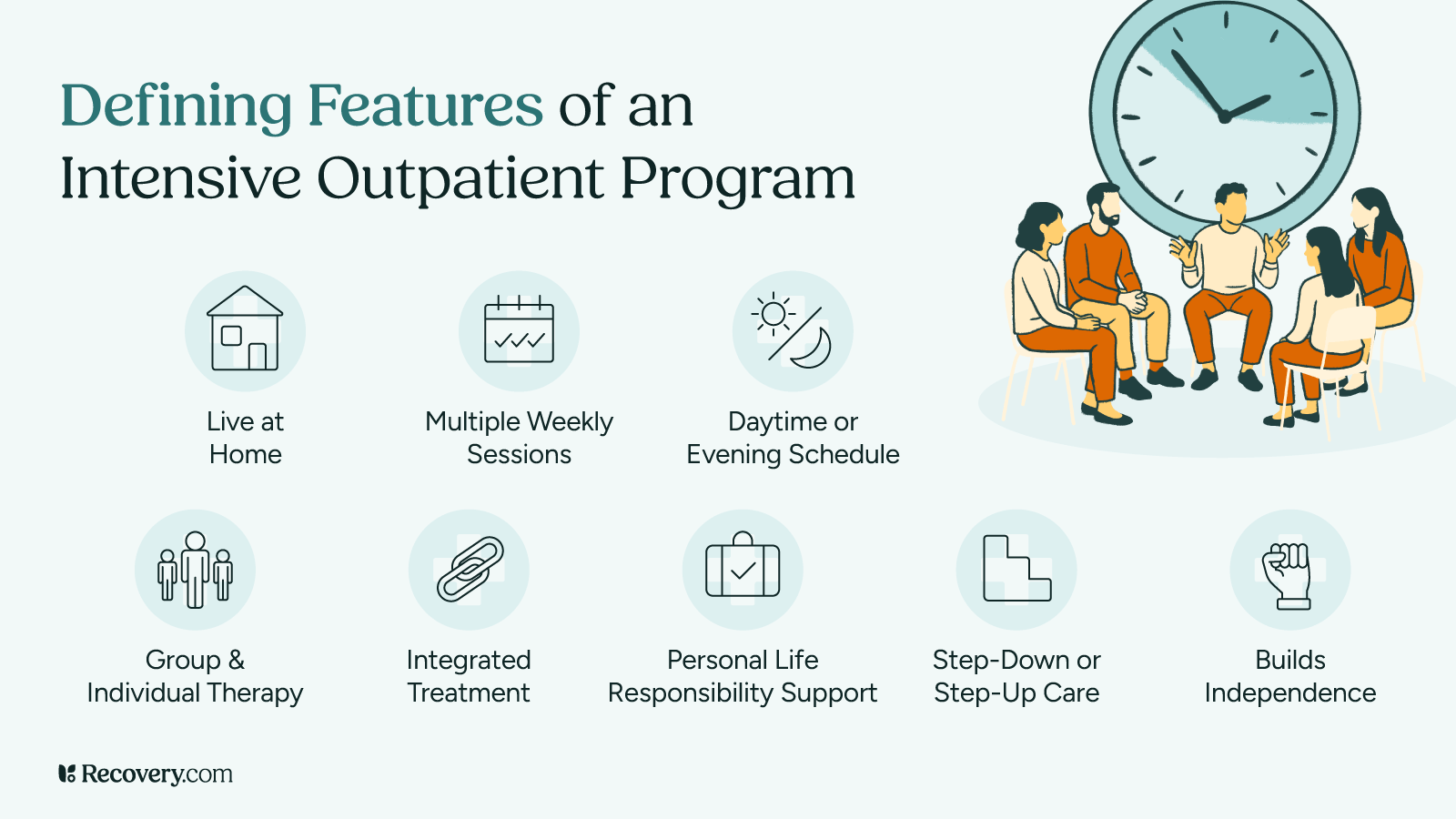
Designed for those who require more than standard therapy but may not need round-the-clock supervision, IOPs offer a unique blend of clinical support and flexibility, empowering people in recovery to integrate their healing into everyday life.
What Is Intensive Outpatient Care?
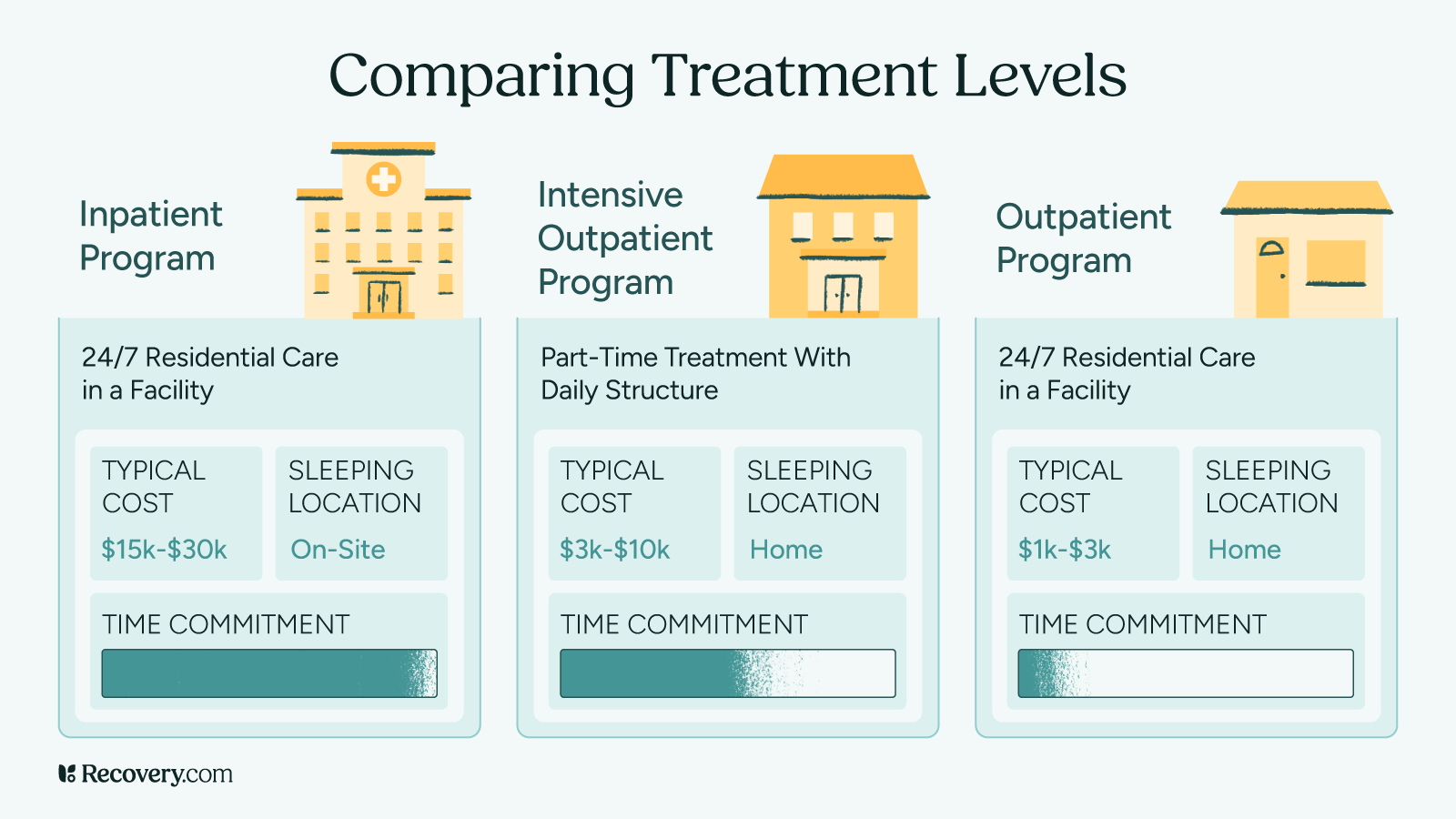
Intensive outpatient care (IOC) is a type of treatment program for people dealing with mental health problems, addiction, or both at the same time. Behavioral health experts rank it as a “Level 2” treatment option,1 which means it provides more support than regular therapy but less than staying in a hospital or treatment center full-time.
This program is structured, meaning it follows a clear schedule and plan. It’s designed to help people who need more help than what they’d get from seeing a therapist once a week, but who don’t need to stay overnight at a treatment facility.
Unlike traditional outpatient programs, which typically involve fewer weekly sessions, IOPs provide a higher level of care2 with several hours of therapy and support each day, often multiple days a week. This approach is suited for those who don’t require a full-time inpatient program or residential treatment but still need substantial support to address their mental health and substance use challenges.
IOPs accommodate a range of needs, focusing on both mental health and substance use disorders, including co-occurring diagnoses. People in these programs take part in different types of therapy. This might include one-on-one counseling, group therapy sessions with others facing similar challenges, and learning new ways to think about and handle problems. One of the best parts is that people can try out what they learn in their everyday lives—at home, work, or school—while still getting support from their treatment team.
This comprehensive approach allows individuals to receive personalized treatment while maintaining their daily responsibilities, fostering resilience and promoting long-term recovery.
Who Can Go to an IOP?
Just like other types of treatment, people need to be a good fit for an IOP program to get the best results. This type of behavioral health care isn’t right for everyone, and that’s okay. Here are some things treatment providers look for when deciding if someone is ready for an IOP:3
- There’s little risk of acute intoxication or withdrawal.
- If you have any physical health conditions, they’re manageable and won’t distract from participation in treatment.
- You can manage your mental health symptoms without staying in a hospital, but you still need regular check-ins. You might have trouble focusing on treatment sometimes because of depression, anxiety, or other concerns.
- Your motivation to get better goes up and down. You need the structure of meeting several times a week to stay on track with your recovery.
- Without regular support, you’re likely to start using substances again or have other problems. Meeting throughout the week helps prevent setbacks.
- Your home life or daily environment isn’t very supportive of your recovery. But with the extra help and structure from an IOP, you can learn to cope better.
Explore Intensive Outpatient Program Treatment Centers
How Does an IOP Help With Addiction Recovery?
IOPs play a critical role in addiction recovery by offering a structured, supportive environment where individuals can receive comprehensive health services while maintaining their daily responsibilities.
The IOP framework is designed to facilitate recovery through a progression from detoxification to discharge, addressing the unique needs of each participant based on the substances involved.
Starting After Detox
While IOPs don’t provide detox services, they often serve as a bridge for people who have already undergone detoxification in a medical facility. For example, someone recovering from alcohol addiction may have completed a medically supervised detox to manage withdrawal symptoms safely. After detox, they step down to outpatient services where they can begin addressing the psychological and behavioral aspects of their addiction.
Getting Your Personal Treatment Plan
Upon entering an IOP, participants undergo a thorough assessment to identify their specific needs, including co-occurring mental health disorders or trauma. For instance, a person struggling with opioid addiction may also have untreated anxiety or depression. This assessment helps clinicians craft a personalized treatment plan that targets both addiction and any underlying issues, ensuring a holistic approach to recovery.
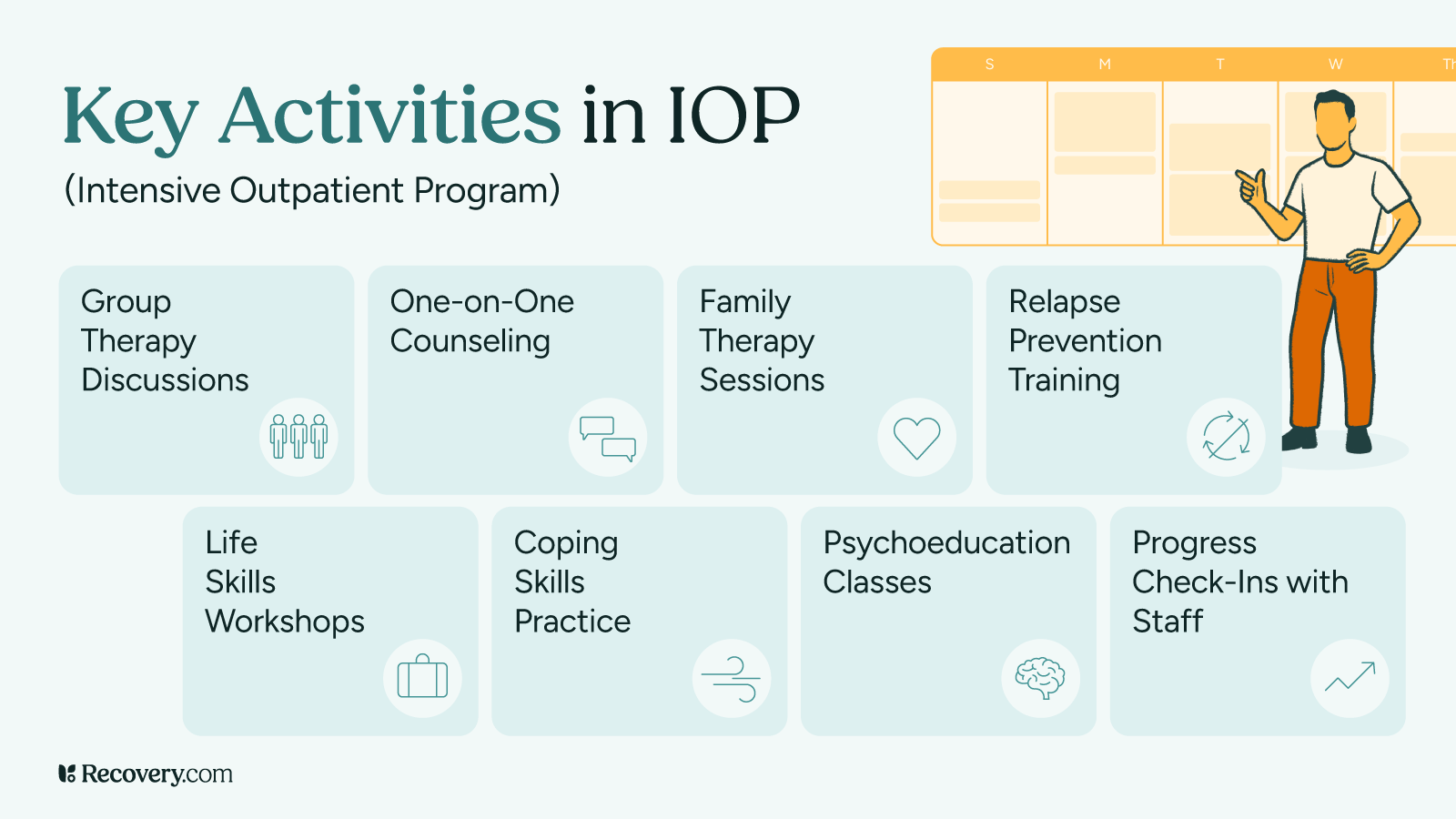
Types of Therapy You’ll Receive
IOPs offer different types of psychotherapy to help you heal. You might take part in individual therapy, group sessions with others who understand what you’re going through, or family counseling to improve relationships at home. Many programs also use DBT (dialectical behavior therapy) to help you manage intense emotions and improve relationships.
In these sessions, you’ll learn about your condition through psychoeducation, discover new ways to cope with stress, and figure out how to avoid setbacks in your recovery.
Medication Management
Many IOPs also include medication management with a psychiatrist or psychiatric nurse practitioner. If you’re taking medications for mental health conditions like depression or anxiety, or if you need medication-assisted treatment for addiction, your treatment team will monitor your medications and make adjustments as needed.
Learning Life Skills for Recovery
Besides regular therapy, IOPs also teach you important life skills that help you handle stress and stay in recovery. You might attend workshops on managing your money, preparing for job interviews, or learning how to communicate better with family and friends. This training is especially helpful if you’re recovering from alcohol use, since drinking often creates problems in your personal relationships and work life that you’ll need to rebuild.
Getting Your Family Involved
Many IOPs encourage your family to be part of your treatment because having people who support you is really important for recovery. In family therapy sessions, you and your loved ones can work through relationship problems and help your family understand how addiction affects everyone. This creates a more supportive environment at home for your recovery. This approach helps no matter what substance you’re recovering from—whether you need to work on family issues related to marijuana use or rebuild trust after using opioids.
Building Your Support Network
As you move through the program, the focus shifts toward planning for when you finish the program and building a recovery plan you can stick with long-term. Throughout your time in the program, you’ll be encouraged to join a support group like Alcoholics Anonymous (AA) or a non-12-Step group like SMART Recovery to build a strong support network outside of treatment.
Continuing Support After You Finish
Finally, as you near the end of your IOP, your treatment team will create an aftercare plan to make sure you have ongoing support and help prevent setbacks. Follow-up sessions, whether through regular therapy appointments or continued participation in community support groups, help you stay connected to your recovery and give you the tools you need to handle life’s challenges after treatment ends.
IOPs give you a complete approach to addiction recovery, helping you through every step from getting clean to finishing the program. By offering treatment that’s tailored to your specific needs, different types of therapy, life skills training, family support, and planning for after you finish, IOPs help you build a strong foundation for lasting recovery. The best part is that you can work on your recovery while still taking care of your responsibilities at home, work, and in your social life.
How IOPs Help With Mental Health and Addiction (Co-Occurring Disorders)
Often, people dealing with both mental health issues and addiction find that IOPs work better for them than regular weekly therapy.4 This is because IOPs offer more frequent sessions and stronger support. When someone has both addiction and mental health problems at the same time, clinicians call these co-occurring disorders (formerly known as dual diagnosis).
Many people start using drugs or alcohol to cope with difficult experiences like trauma, depression, or anxiety. Without treating both the addiction and the mental health issues together, people often get stuck in a painful cycle: they use substances to feel better, then feel guilty or sick afterward, which makes them want to use again.
Here’s how IOPs can help if you’re dealing with addiction along with mental health conditions:
1. Complete Treatment for All Your Needs
IOPs use a team approach that includes evidence-based therapies such as cognitive behavioral therapy (CBT) that are specifically designed to help with co-occurring addiction and mental health disorders.2 You’ll work through your experiences and learn new ways to cope with difficult feelings and situations.
2. Consistent Support When You Need It
Regular sessions give you steady support and a safe place to practice new coping skills. This consistency is really important when you’re dealing with conditions like PTSD and anxiety, as it helps you manage symptoms and navigate triggering situations.
3. Learning Skills That Actually Work
You’ll learn relapse prevention skills to handle symptoms of trauma and anxiety disorders that can trigger substance use. These might include mindfulness exercises, grounding techniques to stay present, or new ways to think about stressful situations. These skills help you become stronger in your recovery.
4. Support From People Who Understand
Connecting with others who have been through similar experiences creates a supportive community. This helps you feel less alone and gives you a safe space to talk openly about your challenges in recovery.
5. Preventing Setbacks Before They Happen
IOPs help you identify and work on the root causes of both your addiction and mental health issues. You’ll learn to recognize and manage triggers that might lead to substance use or worsen your mental health symptoms.
6. Healing Your Whole Self
Many IOPs also offer wellness-focused therapies like art therapy or yoga, which can be especially helpful when you’re dealing with the emotional and physical effects of addiction and mental health issues.
7. Treatment That Fits Your Life
IOPs are flexible, so you can keep up with your daily responsibilities while getting intensive support. This makes it easier to fit treatment into your life and reduces stress that might make your anxiety and PTSD symptoms worse.
Length of IOP Programs
IOPs typically vary in length5 depending on your needs, the structure of the program at your specific treatment facility, and your treatment goals. Most programs last anywhere from a few weeks to several months, depending on what you need:
- 4–6 weeks: Some IOPs are designed for people who need shorter-term support. You might attend 3–5 sessions per week, with each session lasting about 3 hours.
- 8–12 weeks: Many IOPs last 2–3 months and offer more thorough treatment. You might go 3–5 days a week, with sessions lasting 2–4 hours each.
- Longer programs: Sometimes IOPs can last longer than 3 months, which helps you slowly transition to less intensive care. Over time, you might attend fewer sessions while still getting ongoing support.
Choosing a Program
When you’re thinking about an IOP, here are some important things to consider:
- Your recovery goals: Think about what you want to achieve in recovery. This can help you and your treatment team decide how long your program should be and how intensive it needs to be.
- Your availability and commitment: Be honest about whether you can stick to the program’s schedule and requirements. Your success depends on showing up consistently.
- Your support at home: Having family and friends who support your recovery can make a big difference in how well the program works for you.
- Other mental health issues: If you’re dealing with mental health problems along with addiction, you might need a longer or more intensive program to address everything properly.
- Costs and insurance coverage: Check with your insurance to see what’s covered and understand any costs you’ll need to pay out of pocket.
If you’re worried about the cost of treatment, see our complete guide to paying for addiction and mental health care to learn about options that can help make recovery affordable.
Take the Next Step Toward Recovery
IOPs offer a proven path to recovery that may fit into your life while providing the intensive support you need to heal. With personalized addiction medicine, practical life skills, and ongoing support, an IOP can help you build a strong foundation for lasting recovery from addiction and mental health challenges.
If you’re ready to take the next step, find an intensive outpatient treatment program near you that matches your specific needs and insurance coverage. Recovery is possible, and getting started today means you’re one step closer to the life you want to live.
FAQs
Q: What should I expect on my first day of an IOP?
A: Your first day will typically involve paperwork, meeting your treatment team, and getting oriented to the program schedule and rules. You’ll also begin building relationships with other participants and start learning about the recovery process.
Q: Can I work or go to school while in an IOP?
A: Yes, IOPs are specifically designed to fit around your work or school schedule. Many people attend sessions in the evenings or on specific days to accommodate their responsibilities.
Q: What’s the difference between a PHP and an IOP?
A: PHPs (partial hospitalization programs) are more intensive than IOPs, usually requiring 5–7 days per week for several hours each day, while IOPs typically meet 3–5 days per week for 2–4 hours per session. PHPs are better for people who need more intensive support or are transitioning down from inpatient care, while IOPs work well for those who have stabilized but still need structured support while maintaining work, school, or family responsibilities.
Q: What happens if I relapse during an IOP?
A: Relapse doesn’t mean failure or that you’ll be kicked out of the program. Your treatment team will work with you to adjust your treatment plan, possibly increasing session frequency or adding additional support services.
Q: How much does an IOP cost without insurance?
A: Costs vary widely by location and program, typically ranging from $3,000 to $10,000 for a full program. Many facilities offer payment plans or sliding scale fees based on income.
Q: What’s the success rate of IOPs compared to other treatments?
A: Research shows IOPs can be as effective as inpatient treatment for many people, with success rates of 60–80%6 when participants complete the full program and consistently engage in aftercare.
-
“About the ASAM Criteria.” Default, https://www.asam.org/asam-criteria/about-the-asam-criteria.
-
TIP 42: Substance Use Treatment for Persons With Co-Occurring Disorders | SAMHSA Library. https://library.samhsa.gov/product/tip-42-substance-use-treatment-persons-co-occurring-disorders/pep20-02-01-004.
-
“ASAM Criteria.” Default, https://www.asam.org/asam-criteria.
-
McCarty D, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, Delphin-Rittmon ME. Substance abuse intensive outpatient programs: assessing the evidence. Psychiatr Serv. 2014 Jun 1;65(6):718-26. doi: 10.1176/appi.ps.201300249. PMID: 24445620; PMCID: PMC4152944.
-
Center for Substance Abuse Treatment. Substance Abuse: Clinical Issues in Intensive Outpatient Treatment. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2006. (Treatment Improvement Protocol (TIP) Series, No. 47.) Chapter 3. Intensive Outpatient Treatment and the Continuum of Care. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64088/
-
McCarty D, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, Delphin-Rittmon ME. Substance abuse intensive outpatient programs: assessing the evidence. Psychiatr Serv. 2014 Jun 1;65(6):718-26. doi: 10.1176/appi.ps.201300249. PMID: 24445620; PMCID: PMC4152944.
Our Promise
How Is Recovery.com Different?
We believe everyone deserves access to accurate, unbiased information about mental health and recovery. That’s why we have a comprehensive set of treatment providers and don't charge for inclusion. Any center that meets our criteria can list for free. We do not and have never accepted fees for referring someone to a particular center. Providers who advertise with us must be verified by our Research Team and we clearly mark their status as advertisers.
Our goal is to help you choose the best path for your recovery. That begins with information you can trust.







